
[ad_1]
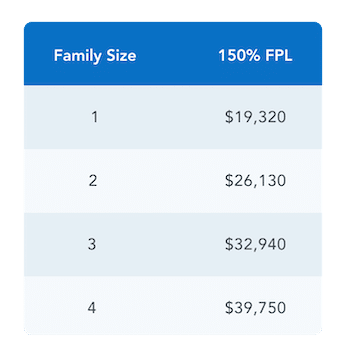
There’s a new Particular Enrollment Interval (SEP) that allows qualifying customers to enroll right into a Market protection for the rest of the 2022 calendar yr. To qualify, the overall family earnings should fall at or under 150% of the Federal Poverty Line. Eligibility relies on the earlier yr’s FPL chart. See chart under for reference.
By this SEP, anybody who match this eligibility can enroll in a Market plan and people already enrolled in a plan can change their plan. In case you are already enrolled in a plan and select to vary your plan, your deductible and out-of-pocket max will reset.
Who’s eligible for this SEP?
Often, customers can apply for a plan at two instances of the yr:
- In the course of the annual Open Enrollment Interval, typically 11/1 – 1/15
- In the course of the Particular Enrollment Interval, 1/16 – 10/31, the place customers sometimes want a Qualifying Life Occasion equivalent to shedding their employer protection, having a toddler, or shifting with a view to enroll in a Market plan.
Throughout this Particular Enrollment Interval, you could be eligible if you happen to fall in each of those standards:
- Have an estimated annual family earnings at or under 150% FPL
- Are eligible for Superior Premium Tax Credit (APTC)* that are a subsidy utilized to your month-to-month premium
*As a reminder: Customers with earnings under 100% FPL however who don’t qualify for Medicaid as a result of immigration standing solely should still be eligible for APTC in the event that they meet all different Market eligibility necessities. They might additionally qualify to make use of this SEP.
Who will not be eligible for this SEP?
Customers have to be eligible for APTC (a subsidy utilized to your month-to-month premium) with a view to use this SEP. Meaning they can’t be eligible for Medicaid or supplied reasonably priced employer-sponsored protection. This additionally means customers who fall into the Medicaid Hole (i.e. make lower than 100% FPL in states that didn’t take part in Medicaid growth) can not use this SEP; nothing about this new SEP modifications their eligibility for subsidies.
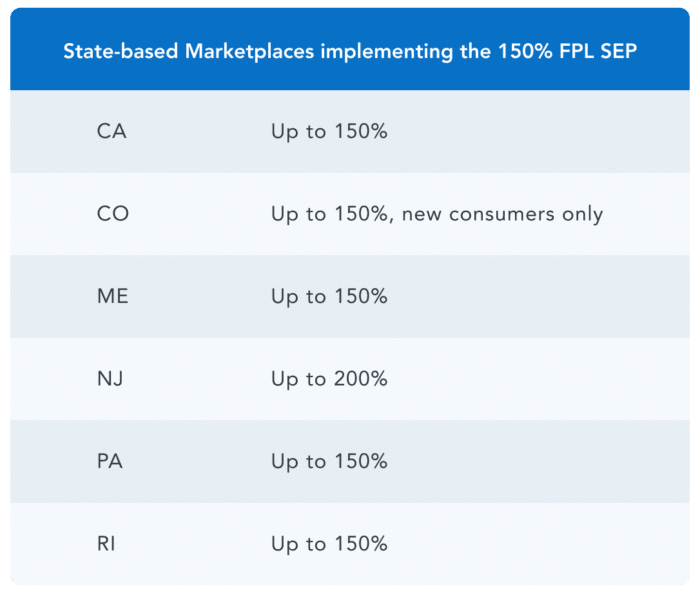
This SEP is stay for the Federally-facilitated Market (FFM) and all plans on HealthSherpa. Implementation of this SEP varies for states that function their very own alternate.
What are the efficient date guidelines?
This month-to-month SEP will comply with accelerated efficient date guidelines, which implies customers can enroll any day of the month and have their protection begin the primary day of the subsequent month. For instance, if a client enrolls in a plan on 3/30/22, their protection will start on 4/1/22.
How will I do know if I’ve obtained this SEP?
After submitting an software, any qualifying applicant of this SEP will see that they’ve obtained the SEP “as a result of estimated family earnings (≤150% FPL)” on the eligibility outcomes web page.
How lengthy will this SEP final?
For now, this SEP solely exists for the 2022 calendar yr. It should solely be prolonged if the American Rescue Plan (ARP) subsidies are prolonged. With ARP subsidies, most customers who’re eligible for this SEP can enroll in free silver plans.
How do I do know if I qualify for this SEP?
To see if you happen to qualify, you can begin a quote by coming into in your zip code under.
[ad_2]